Antidiuretic Hormone (ADH)
Also known as arginine vasopressin (AVP), ADH is a nine-amino-acid peptide
made in the supraophthalmic nucleus (SON) of the hypothalamus. Once made, it
is transported by axons to the posterior pituitary, where it is released into
the bloodstream.

Secretion of ADH to reabsorb water is regulated by two mechanisms.
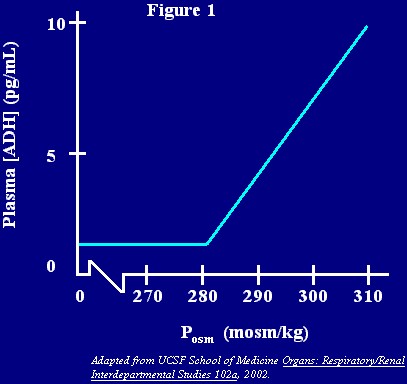
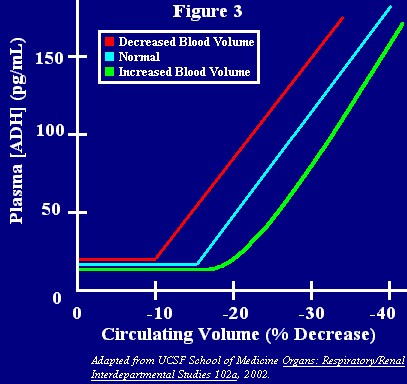
- Osmoreceptors located in the anterolateral hypothalamus
measure Posm. These cells play key roles in water and sodium balance. Changes
in Posm result in cell swelling or shrinking, thus signaling the release
(or prevention of the release) of ADH. At Posm below 280 mosm/kg, these cells
are virtually inactive and do not stimulate ADH secretion. However, small
changes above this Posm (even of only 1%) will trigger major firing changes
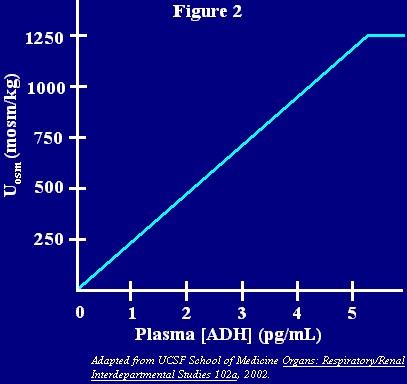
in osmoreceptors (Figure 1). At a Posm of 290 mosm/kg, enough
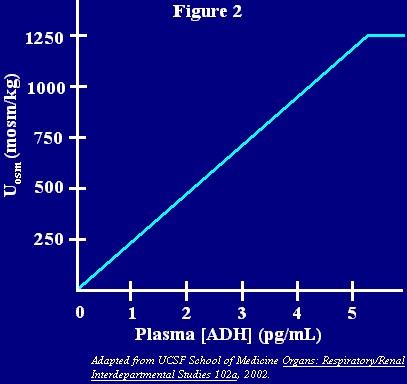
ADH would be secreted (5 pg/mL) to cause a maximum retention of water, yielding
Urineosm of 1250 mosm/kg. Any [ADH] above 5 pg/mL results in this same maximal
antidiuresis (Figure 2). Not all osmotically active substances
can stimulate shrinking or swelling of the of osmoreceptors; while sodium
ions are able to do this, urea cannot since it can freely cross membranes.
In addition to regulating release of ADH, osmoreceptors also regulate thirst
with a relationship similar to that shown for ADH in Figures 1 and 2.
- Baroreceptors, located in the carotid sinus and aortic
arch, measure blood pressure. Unlike osmoreceptors, baroreceptors must be
suppressed in order to stimulate the release of ADH; this suppression, in
turn, comes about after a fall in blood pressure. Sensory fibers from cranial
nerve IX (glossopharyngeal) and X (vagus) carry this signal from the sinus
and arch to the ADH-releasing neurons of the hypothalamus.
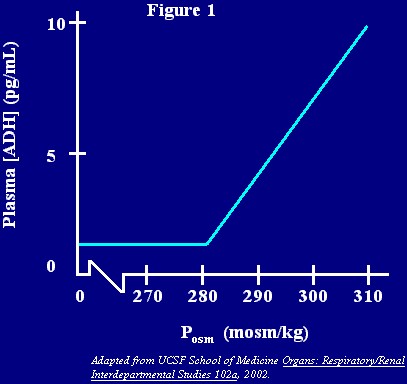
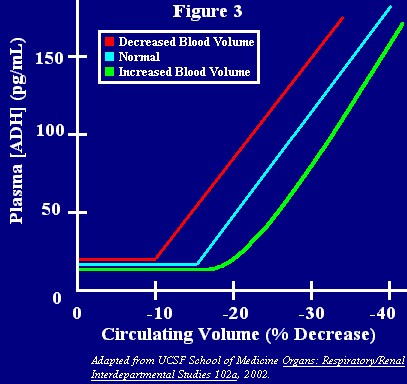
Another difference in the baroreceptors is that larger changes in the dependent
value (in this case circulating blood volume) are needed to release ADH.
Ten to fifteen percent of the blood volume must be lost to result in ADH
secretion (Figure 3). Figure 3 also shows that this threshold
value depends largely on the original blood volume. But the decreased sensitivity
put aside, these receptors have the potential of releasing much more ADH;
this is particularly relevant since ADH acts as a vasoconstrictor at high
concentrations (therefore, these receptors help maintain blood pressure by
increasing peripheral vascular resistance). They can also override osmoreceptor
signals.
Baroreceptors can also stimulate thirst.
NOTE: ADH release is also influenced by [Angiotensin II]
and drugs. Nicotine, ether, morphine, and barbiturates increase ADH release
while alcohol inhibits it.
The table below summarizes the major characteristics of osmoreceptors and
baroreceptors.
| Receptors |
Osmoreceptors |
Baroreceptors |
| Location |
anterolateral hypothalamus |
carotid sinus & aortic arch |
| Value Measured |
Posm |
circulating volume |
| ADH Release Stimulated By |
activation of receptor |
suppression of receptor |
| Change Required for Action |
1% above 280 mosm/kg |
10-15% decrease |
| Resulting Amount of ADH |
small |
large |
| Override Other? |
no |
yes |
Actions of ADH

- Water reabsorption: This action is mediated by ADH interactions
with V2 receptors on the basolateral membrane of collecting-duct principal
cells. Coupled to adenylyl cyclase by a G protien, these receptors lead to
the eventual activation of cAMP-dependent protein kinase A, which increases
water-channel insertion into the apical membrane. The V2-receptor interactions
also increase the collecting duct permeability to urea. As a result, with
ADH present, urea and sodium ion contribute equally to the osmolality of
the medullary interstitium.
Regardless of the mechanism, it is important to realize that ADH only
controls “pure” or osmotically-free water, not solutes.
- Vasoconstriction: This action is achieved at high [ADH]
and is mediated by V1 receptors on vascular smooth muscle cells.
FYI:
Three malfunctions of the ADH system result in noticeable disease. All have
some form of treatment.
- Central diabetes insipidus: This disease is seen when the pituitary
gland is unable to secrete ADH.
- Nephrogenic diabetes insipidus: This disease is seen when the
collecting ducts are unable to respond to ADH due to a mutation in the V2
receptor.
- Syndrome of inappropriate ADH secretion (SIADH): This disease
is seen when drugs or tumors result in continued secretion of ADH or increased
action of ADH on the collecting ducts.
Antidiuretic Hormone Agonists and Antagonists
ADH Agonists
 Two
peptides, ADH and desmopressin, facilitate water reabsorption from the collecting
tubule by cAMP-mediated insertion of water channels there. As a result, both
decrease the volume of urine and increase its concentration.
Two
peptides, ADH and desmopressin, facilitate water reabsorption from the collecting
tubule by cAMP-mediated insertion of water channels there. As a result, both
decrease the volume of urine and increase its concentration.
Clinical Uses: The two can be used for
central diabetes insipidus but not nephrogenic diabetes insipidus. The latter
requires reabsorption of water before it reaches the nonfunctional collecting
duct system. Salt restriction, thiazides, and loop diuretics can partially
achieve this by reducing blood volume and stimulating PCT reabsorption as a
result.
Toxicity: Hyponatremia may result in the
presence of ADH or desmopressin. Hypertension can also result with high doses.
ADH antagonists
ADH antagonists demeclocycline and lithium work at some point after the cAMP
generation, likely by preventing the insertion of water channels
Clinical Uses: The two can be used against
any chemical (like ADH) that acts on the V2 receptor. Tumors or drugs can produce
the V2 agonists and can cause significant hyponatremia. SIADH can be treated
well with demeclocycline; lithium is used less due to its toxicities.
Toxicity: In younger children, demeclocycline
can cause abnormalities in teeth and bone as well as liver and kidney toxicities.
Lithium can cause nephrogenic diabetes insipidus, edema, thyroid function decrease,
and much more.


 Two
peptides, ADH and desmopressin, facilitate water reabsorption from the collecting
tubule by cAMP-mediated insertion of water channels there. As a result, both
decrease the volume of urine and increase its concentration.
Two
peptides, ADH and desmopressin, facilitate water reabsorption from the collecting
tubule by cAMP-mediated insertion of water channels there. As a result, both
decrease the volume of urine and increase its concentration.